BY PAUL SCHINDLER
I am in self-quarantine for COVID-19.
Is that because I know I’ve had an exposure to the coronavirus? No, not for certain. And that uncertainty speaks to how crippling the current state of this pandemic is for the way we carry on our daily lives.
A co-worker of mine has experienced five days of high fevers, chills, a cough, and periods of labored breathing. He’s been exhausted but has been so uncomfortable at times that he’s been unable to sleep.
Thankfully, he’s feeling better today and it looks like he’s on the mend.
But here’s something that’s a damning indictment on our healthcare system and our government’s response: he has been unable to get tested for COVID-19.
His doctor told him he “definitely could” have the coronavirus, but said he can’t be tested at this time. Still, the doctor referred him to an urgent care center, which in turn told him to call the New York State coronavirus hotline. There, he was told that our local public health resources lack the capacity to give him a test given the symptoms he described.
That answer was not surprising since the city health department last night tweeted, “Testing should only be used for people who need to be hospitalized for severe illnesses like pneumonia.”
By now, we’ve all seen the reporting on the failure of the federal government to have emergency health crisis preparedness in place — what with the president’s dismantling of that unit in the White House National Security Council — and on the ham-handed rollout of testing and the continued red tape hobbling our ability to expand its capacity. Many other nations — some considerably less affluent than our own — are doing far better on this score.
The nation’s testing failure — as no less than Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, termed it to Congress last week — puts the primary burden for limiting the virus’ explosion onto each of us.
In a New York Times op-ed over the weekend, Charlie Warzel wrote compelling about the whys and hows of that. He pointed out that even though millions of workers were doing their jobs remotely from home to avoid infection, many were spending their evenings in restaurants and bars. Perhaps young and/ or healthy, they may have also felt invincible. But as Sanjat Kanjilal, of the Harvard Pilgrim Health Care Institute’ Department of Population Medicine, has pointed out, epidemiological “modeling suggests that the impact of distancing among low-risk people is more important to decrease transmission than its impact for high-risk people who move around less.”
In other words, it’s not just sick people, old people, and others whose health makes them particularly vulnerable to the coronavirus that need to avoid social contact in large groups. Everybody has to. Because even if you’re healthy and feel fine, you might be carrying the virus and spread it in large groups or might contract it and spread it elsewhere.
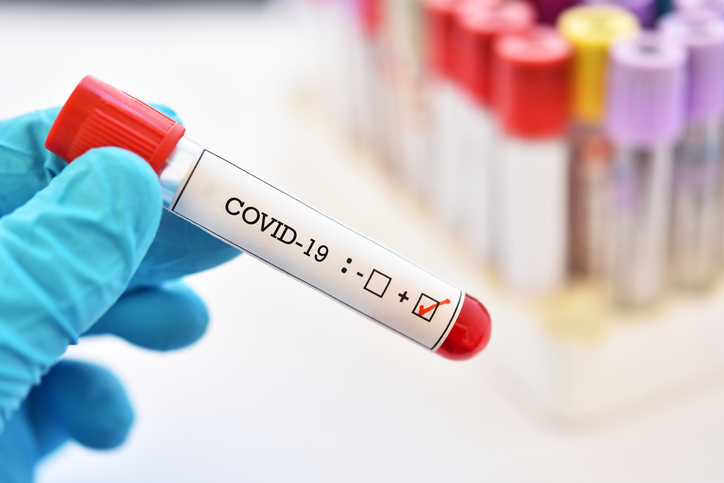
That was the logic behind New York City and other localities closing restaurants, bars, and other entertainment venues.
But it’s not enough for us to abide by the rules government is setting. We need to apply them in our own lives.
So for the time being, don’t bring the party home. Exercise prudence in your social interactions. Check in on vulnerable people in your lives. And should you become ill, be responsible about reporting that to those you’ve recently spent time with.
These guidelines provide the best route to flattening the curve on infections across the nation. Public health is a community effort.