The NewYork-Presbyterian hospital network announced a new wave of visitor restriction policies over the weekend due to the coronavirus crisis. The in-patient guidelines include the blanket barring of visitors for any adult inpatient, with perhaps the most shocking of the restrictions being the exclusion of birth partners for laboring women.
A statement by the 13-hospital network read, “We understand that this will be difficult for our patients and their loved ones, but we believe that this is a necessary step to promote the safety of our new mothers and children.”
The restrictions will also be implemented at affiliate Weill Cornell and Columbia hospital networks across the city.
Women who have been admitted to labor and delivery suites will be tested for COVID-19 regardless of symptoms and will be forced to wear masks.
These updated visitation policy changes were released one week after an initial rollout of stringent guidelines detailing the postponement of all elective surgeries and reducing the number of birth partners able to attend deliveries to one.
Also stated in the release was the following mediation strategy: “We encourage visitors to remain closely connected to their loved ones through virtual means, including Skype, FaceTime, and/or phone.”
Patients who do not have access to such technologies were not discussed.
This move by NewYork-Presbyterian is completely unprecedented, even within the current “epicenter” of the virus, Europe. In the past few weeks, hospitals in the UK have recommended birth partners wear masks, wash their hands thoroughly and do not leave the delivery suite until labor has ended and the newly formed family is discharged.
Even extremely hard hit hospitals in England that are banning visitors from inpatient wards unless there are “exceptional circumstances,” have retained visitation rights for birthing partners, highlighting laboring women as a unique patient population with specific needs.
A birth partner can be an aide in these times when healthcare workers are stretched thin. For example, should a laboring woman have a seizure, or faint, a birth partner may be able to sound the alarm should overworked staff members be absent.
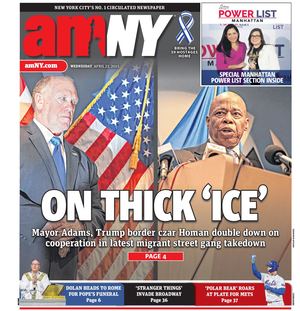
The American College of Obstetricians and Gynecologist’s Vice President of Practice Activities, Christopher Zahn, MD, released a statement to amNewYork Metro on March 23 which balanced the need for caution in hospitals with recognition of the fact that “continuous one-on-one emotional support provided by a partner or support person such as a doula is associated with improved outcomes for women in labor.”
Examples of such improved outcomes were discussed in a Cochrane Systematic Review on “Continuous Support for Women During Childbirth,” published in 2013.
As well as increasing a woman’s satisfaction with childbirth, the presence and continual support of a birthing partner had the following, statistically significant benefits: women were more likely to have a spontaneous vaginal birth, had shorter labors, were less likely to have a caesarean section or instrumental vaginal birth, rely on pain medications or birth a baby with a low five-minute Apgar score—a test used to determine how well the baby tolerated the birthing process and how well the baby is doing outside of the womb.
In guidance issued as recently as March 18, the World Health Organization described a safe and positive childbirth experience as one that categorically includes the right to have “a companion of choice present during delivery.”
No official from NewYork-Presbyterian was available for comment as of press time.