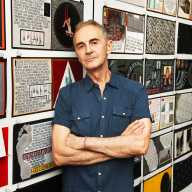
Michael Fosina, C.E.O. of New York-Presbyterian/Lower Manhattan Hospital.
BY DUSICA SUE MALESEVIC | Change is afoot for Lower Manhattan’s only hospital — and the community is taking notice.
After struggling New York Downtown Hospital merged with NewYork-Presbyterian 18 months ago, some people feared cutbacks, but instead, new services and more staff have been added as well as an almost $20 million ongoing renovation of its fourth floor.
“Now since Presbyterian [took over] it’s a different day,” John Fratta, chairperson of Community Board 1’s Seaport Committee, said in a phone interview. “We finally have a hospital that we can utilize.”
“Beekman” was one of the worst hospitals and was poorly staffed, said Fratta, referring to one of the hospital’s former names.
He has been to the hospital on three recent visits and said that he has “nothing but compliments.”
Michael Fosina, the hospital’s head, took Downtown Express on a tour Dec. 4 of NewYork-Presbyterian/Lower Manhattan Hospital that includes parts that have been upgraded and changed as well as the new wing, which is currently under construction.
“It’s an exciting new project for us and the hospital,” said Fosina, senior vice president and C.E.O. of Lower Manhattan Hospital. “We’re starting to piece it all together.”
The complete makeover of the fourth floor began almost as soon as the two hospitals merged on July 1, 2013. The floor was gutted and is now being shaped into several rooms, an entrance and nursing stations.
The new patient rooms will also include features such as a board that will list all pertinent information about the staff administering care.
Currently, the hospital has 132 beds and when the new floor is open in April of next year, 20 more beds will be available. (New York Downtown Hospital at one time had 254 beds in 2006; it had 180 in 2013.)
In the emergency room, there is a new separate section dedicated to pediatric care and a pediatrician is on duty 24 hours a day.
When St. Vincent’s Hospital was about to close in 2010, the Downtown community was concerned about the lack of pediatricians available at Lower Manhattan emergency rooms. CB. 1 wrote letters urging St. Vincent’s to stay open and cited this as one of the reasons.
“This is great,” said C.B. 1 chairperson Catherine McVay Hughes, who pointed out the community’s growing youth population. “It’s filling a huge gap since St. Vincent’s has closed.”
Fosina said that the adult emergency room has been streamlined and the hospital has been working on being more efficient so people can see a doctor faster.
The William St. lobby is also being redone, explained Fosina, and should be completed by February. There are plans to overhaul the operating room, labor delivery and postpartum units and the hospital’s procedure areas.
“The whole interior of the building will eventually get done,” he said. “It’s going to take us years to do that because you got to live in the space at the same time that you’re doing renovations, which is complicated.”
In addition to hospital’s physical changes, Fosina said more staff and services have been added and expanded.
“We’ve been adding more physician services,” said Fosina in his office that had shelves lined with football helmets and baseballs. “We brought more specialty services down here,” including neurology and gastroenterology.
“Lower Manhattan needed a place for residents to get healthcare,” he said. “It needed a stable place. This is the only hospital south of 14th St. We felt that it was the right opportunity to have us come down here and help stabilize and expand access to healthcare in the Lower Manhattan community.”
Through its history, Lower Manhattan Hospital has gone through several name iterations. Prior to 1991, it was Beekman Downtown, then New York Infirmary-Beekman Downtown Hospital, then N.Y.U. Downtown Hospital and finally New York Downtown Hospital. Before this recent merger, the hospital has been plagued with financial difficulties.
New York Downtown Hospital was associated with New York University until 2005. After that it was independent, although it did have ties to NewYork-Presbyterian before the merger.
Fosina was in charge of the transition and said he was chosen because NewYork-Presbyterian wanted someone who understood the organization and how it works.
For over 20 years, Fosina has worked for the NewYork-Presbyterian and at almost all of the six different locations. Before coming here, he was running Allen Hospital, which is at the northern tip of Manhattan.
New York Downtown Hospital had a different culture, Fosina noted when asked about the challenges of integrating two hospitals. It was an independent hospital, he said, and he is moving to make it part of the NewYork-Presbyterian system.
“We want the same level of care, the same level of service, the same level of experience at this campus as we do all of our campuses,” he said. “We continue to integrate and change culture.”
Lower Manhattan is turning into a full-service hospital, said Fosina, which is responding to community needs. For example, the special children’s area of the emergency room was created because there are so many families down here, Fosina explained.
There has been a growth in the amount of people using the hospital, according to Fosina, who said that on the surgical side there has been about a six percent increase in patients.
NewYork-Presbyterian is affiliated with Weill Cornell Medical College and if a patient needs treatment that is not available at the hospital, they can go to one of the academic medical centers. Fosina said the patient’s care will be seamless because of the close relationship.
Fosina grew up in Westchester and after attending the University of Delaware for a bachelor’s degree in animal science, he got a job at Columbia University’s cardiology department as a technician. While at Columbia, he took a class in hospital administration and became “completely fascinated.” He ended up with a graduate degree from the university’s school of public health.
“It is about the health of the public,” said Fosina, who now lives in New Rochelle. “It’s about the health of the community. Hospitals are supposed to be trusted resources in the community and it’s an opportunity to really give back to the community in a meaningful way.”
The hospital has reached out to the community board, said Fratta, and given members two tours of the facility.
“We’re very pleased,” he said.
Fosina has gone to Community Board 1 meetings for updates and said that the hospital, which has sponsored events, truly wants to be a community partner.
“Hospitals need to be trusted resources in the community. That’s why we’re here,” he said. “The community needs to be comfortable and know that we’re here for them in their time of need.”