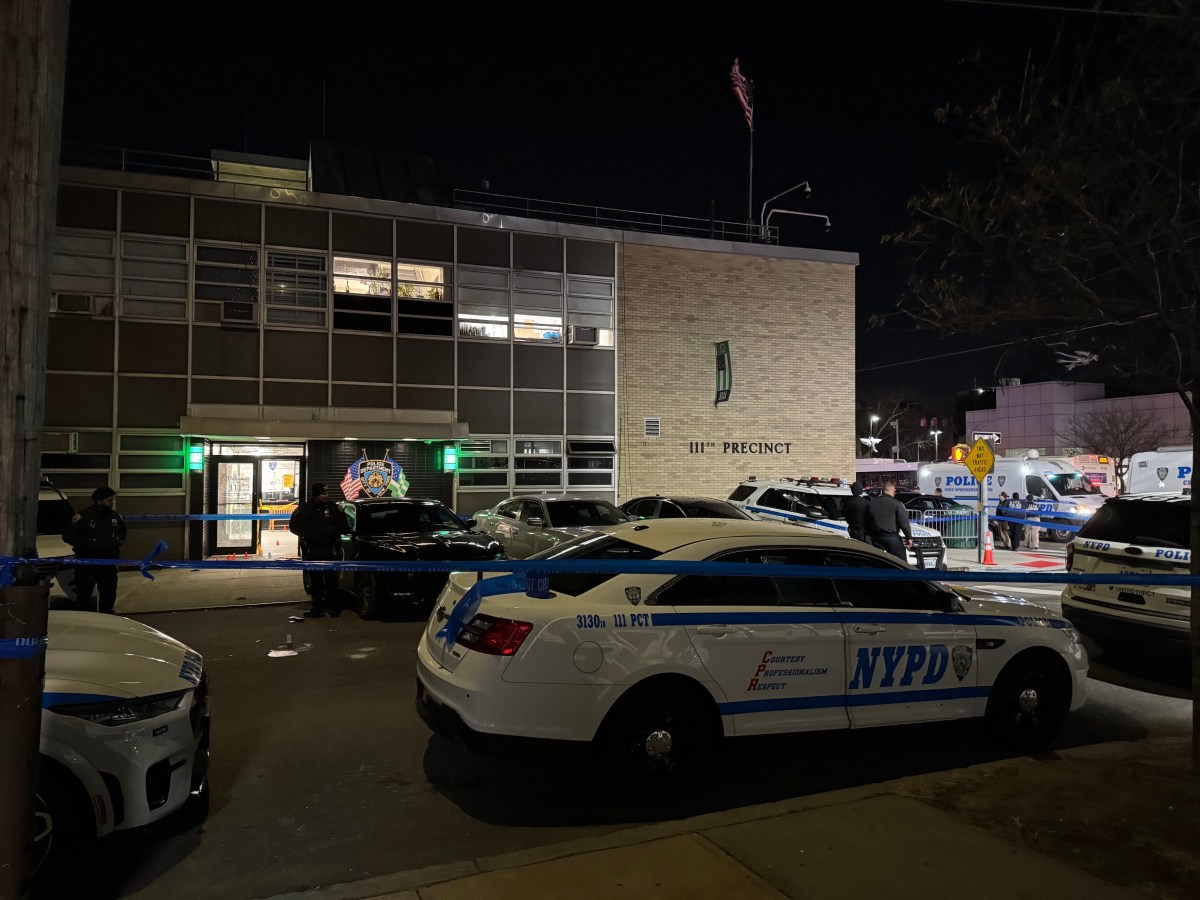
New York City’s B-HEARD teams (Behavioral Health Emergency Assistance Response Division) aim to change the way the city responds to mental health emergencies by sending social workers and FDNY paramedics in to assist and help calm troubled individuals.
Recently, Mayor Eric Adams announced an expansion of the $43 million B-HEARD program, which was first launched in June 2021. The city plans to add two peers — individuals who have personal experiences living with a mental health condition — to every mobile crisis team.
The B-HEARD program is active across Harlem, Washington Heights, Inwood, the South Bronx, Brownsville, and East New York. The program is currently hiring for licensed social workers in Manhattan, Brooklyn, and Queens.
B-HEARD teams, comprised of two EMTs and a social worker from NYC Health + Hospitals, respond to a range of mental health emergencies that might involve people experiencing suicidal ideation, serious mental illnesses, substance use, and behavioral and physical health problems. Teams are on the streets 16 hours a day, seven days a week, from 9 a.m. to 1 a.m.
In its first full fiscal year of operation, B-HEARD responded to 73% of calls routed to them from 911 calls, totaling roughly 1,700 calls.
The city has made it clear that police, rather than B-HEARD teams, respond to calls where patients need to be immediately transported to a hospital, where someone has a weapon or is presents violence, located in a difficult-to-reach area such as a bridge or in traffic, or showing suicidal behavior — essentially situations where someone presents a “risk of imminent harm to themselves or others.”
amNewYork Metro recently sat down with three of B-Heard’s workers to learn more about their jobs and how they respond to New York City’s mental health emergencies.

Morgan Nevins, Licensed Social Worker in the South Bronx division
Tell me about your daily work with the B-Heard program.
I work on our day shift. We have an EMS station house where we meet our EMS partners and social workers on my shift. From there, we see which truck I am on. We gather our radios, equipment. We log on to the dispatch system showing our unit and the 911 dispatch system is available and ready to respond to calls.
Sometimes I’ll get a call as we clock in at nine. If we don’t get a call right away, we’ll head towards our designated parking area in the community, which FDNY determines would be the most centralized location for us to respond the fastest. In the Bronx, we cover a few different precincts. We have multiple trucks running. People can also approach our truck in need of support.
We have people who call 911 reaching out for support for the first time. They do not have a history of receiving mental health services. They never had a therapist before and might be experiencing suicidal thoughts for the first time and be afraid.
I’ve responded to people of all ages from seven to 70, of all backgrounds, abilities, and identities. Something I see often on our shift is calls for young people: children, adolescents, and young adults experiencing acute mental health crisis. By acute, I mean someone calling 911 in crisis. They are experiencing something very intense in that moment. Since the pandemic, young people are facing a lot of mental health challenges and requiring support.
What are your goals while on the job?
I was invested in being a part of a culture shift in emergency response and exploring how B-HEARD was working on the ground. When I applied, they were hiring for the South Bronx, an area I feel like there is a lot of need. Previously a traditional 911 response includes a mix of EMS and police. We are shifting that and bringing mental health practitioners to people at the entry point of a 911 emergency.
This is a patient-centered, health-centered, more public health-oriented response. We are taking into account this person’s medical and mental health status in that moment. We provide support to people on the street, schools, shelters and supportive housing, mental health and medical clinics, and in their apartments.
Medical conditions and mental health are often interrelated, so that’s why it’s a perfect marriage between EMS and social work. We provide this person an opportunity to feel listened to, to have ownership in their care, and provide them with alternatives, where appropriate, to the hospital. While the hospital has a very important role in our community, it might not always be the best fit, depending on the nature of the crisis. Ultimately our goal is to avoid an additional or future 911 crisis.
What experience do you bring with you?
My first job after social work school was mobile crisis. I provided crisis support and counseling, mental health triage assessments for people who might have been discharged from the hospital and were referred to therapy, or someone to follow up for therapy appointments, or to see if they had adequate services.
I am a sibling of someone who has a disability. I have worked in domestic violence, sexual assault, and human trafficking advocacy, (and) in emergency shelters for survivors. I’ve worked with people who are living with HIV in a variety of settings in the United States and outside of the United States. I’ve worked in community health work, doing home-based care visits for people who have chronic diseases.
When I became a social worker, I was interested in what a trauma-informed, anti-oppressive approach might be to clinical social work practice. I’ve had a long and winding road to finding my fit as a social worker, but I feel very lucky to come to work every day with B-HEARD.
Give me an example of what an emergency call has looked like.
There was a call I responded to with a middle-aged woman having expressed thoughts of suicide. The 911 call was made by the housing case manager. When we arrived on scene, we met with this woman in her supportive housing apartment. We had a discussion with her about what what she was feeling. She reported having thoughts of jumping out a window because she had a lapse in her benefits (and) medical insurance. She had gone months without a therapist, without her medication, and her necessary benefits. She had become very exasperated at the administrative errors blocking her from getting adequate care.
We developed a safety plan with her to navigate the anxiety, frustration, and distress she was under. Her heart rate had gone down over the course of the interaction. I was able to refer her to a city program through the mayor’s office for crisis response where a team of social workers connect with her in 24 to 48 hours. After I submitted the referral, they were able to work with her and her housing case manager to address the lapse in benefits.
What have you learned about the city’s mental health crisis during your time at B-HEARD?
What feels safe to me, as I physically present as a white woman, might not feel safe to other people. It’s a beautiful thing when we walk into a scene and have someone be upset that 911 was called and might not want to engage with us, find out this person seems to care about what I want and need in this moment. Taking that time to hear them out and collaborate with them can get to the root of the problem over the course we’re there. I have been in jobs where things might have shifted, and although I might have felt concerned, I never doubted that me and my partners would be able to navigate that situation and get home safely.
Sedicah Powell, Bronx Borough Coordinator
Tell me about your daily work with the B-HEARD program.
I work half of the week administratively and the other half in the field as a social worker. I’m in meetings with FDNY to talk about the overall operations (and) to ensure we have adequate staffing for our trucks. I conduct meetings with staff to talk about cases they’ve encountered in the field and to give them guidance on how to handle certain situations. I usually spend the rest of the day in meetings where we talk about our clinical practices or things we want to implement for B-HEARD.
The other half is doing everything the social workers do. We receive and respond to 911 mental health calls as quickly as we can. We go on calls where units requested a police presence for backup and support. When we arrive on scene, first we want to make sure the scene is safe not just for us, but also for whatever’s happening for the patient, whether it’s in their home (or) on the street. We figure out who called 911 to get some information from that person (and) from anyone else on the scene.
Then just approaching the patient and trying to engage in rapport building. Asking: “Can you talk to me about how your day has been today? Has there been anything particularly difficult for you? Have you been able to enjoy your typical activities? Or is there something that’s giving you a hard time today? We work as a team to strategize and help de-escalate and figure out the best outcome for this patient in their moment of crisis.
I’m motivational interviewing and repeating back to them and offering some guidance or assisting with an outcome: “It sounds like you’ve had a rough time today. Maybe you should separate from this person who appears to be making you upset.” Sometimes people don’t think of those things in the moment. We have been getting a lot more disputes; usually it’s one person arguing with another person. We have different cases, but these de-escalation techniques are applicable to different scenarios.
What experience do you bring with you?
I am a licensed master social worker. Prior to joining B-HEARD, I used to be the assistant director of care coordination through (NYC) Health + Hospitals for about three years. Prior to that, I was the clinical supervisor in supportive housing where we worked with individuals who had serious mental illness to assist them with access to resources and making sure they have help with their activities on a day-to-day basis. I’ve also worked in inpatient psych in many different areas, as well as a social worker throughout New York.
What are your goals while on the job?
My personal goal for the program is to strategize ways to work with our EMS or FDNY partners, to expand the program, to increase our call volume, to onboard new staff, to provide training and education. The whole premise of the B-HEARD program is to give people options when they’re in crisis, to give people alternative support to what they’re already receiving. This is something that’s so unique and so different for our city.
What are your greatest challenges while on the job?
Some of the challenges can be seeing somebody going through a tough time or crisis and not feel well equipped. You’re passionate about helping them, but sometimes you’re working with this individual who may not see that for themselves. Another challenge can be trying your best to offer the right suggestions, ideas, and solutions to someone you just met.
Salley May, Social Work Supervisor for Harlem and Bronx units
Tell me about your daily work with the B-HEARD program.
As a social work supervisor, direct supervision of the social workers. Right now we have three social workers who work during the day and four social workers who work our evening shift. We have a supervisor during the day as well as another supervisor joining our team shortly. We don’t supervise the EMTs and the FDNY staff, but we’re always educating each other.
I oversee what’s going on clinically in the field. I’m usually covering a truck myself, (which) means you are the primary clinician. We respond in what looks like an ambulance outfitted to have a social worker in the back. We don’t transport patients, we call another unit to transport a patient if they need to go to the hospital.
First thing is showing up: Let’s get the trucks out. We want to go into service as quickly as possible. We go to “89,” which is a zone of accepting calls (and) jobs. We get a call, a text and we respond and stay on scene until it’s clear what needs to happen. Often it’s making collateral phone calls to providers or family. It’s educating the family in Spanish and English. We’re working to have other languages.
The critical thing is we don’t leave them in crisis without having a safety plan for them. We have also what’s called a HEAT team that will contact that patient within 24 hours and put things in place for them.
What experience do you bring with you?
I have 20 years of experience on Bellevue’s mobile crisis team going to people’s homes (and) to shelters and doing assessments, and in the psychiatric emergency room at Bellevue Hospital.
I came to New York from California where I was a substitute teacher in Watts. I jumped into theater, dance, visual art workshops with people with mental health challenges, hospital audiences, (and) disadvantaged populations.
I’m bringing years of experience of being able to look at a situation and to pretty accurately assess the level of risk. That is the important piece in determining what we can do for that patient.
What are your goals while on the job?
Our program is about finding other resources if they don’t need to go to the hospital. Often, we find there is acute crisis and a person needs to go, but we have been successful in managing to reduce the number of unnecessary hospital transports. It has everything to do with the level of risk they may be at that time. If they are acutely suicidal, if they want to harm themselves, they need to be in a safer environment so we take them to the hospital. If they are acutely psychotic and have paranoia that people are after them, that’s not a safe way to be in the community. We take them to a hospital. If however, they feel depressed and need some support, they don’t need to be in a locked environment.
If police are not needed, they’re not there. It usually is us and the EMTs. We have access to Support and Connection Center(s). We have one in Harlem and one in the South Bronx. It’s a brief stay. We can bring patients there. Police also are able to separately bring patients there. They can also return on their own. What it offers is immediate support. There are peers, a social worker, a doctor, a nurse. It’s a health-centered response, not a public safety response.
What are your greatest challenges while on the job?
A big need is appropriate housing for people. One big difficulty is having available in-person resources. A lot of things went remote for a long time. Mobile crisis was off the charts through the height of the pandemic. Things really escalated during that period, and I think we’re gonna see the repercussions of what those shutdowns did for everyone.
What have you learned about the city’s mental health crisis during your time at B-HEARD?
The scene is benefited by us being there to de-escalate a patient that might be loud and seem a little scary. The whole scene transforms with us being able to connect with the patient and have the clinical skills through the social worker, and the medical skills and street smarts of EMTs. We want to keep them out of emergency rooms. We don’t want them to go under arrest for an issue that we could help with. It feels like we are solving many issues for people, rather than perpetuating what happens for them over and over again.
Read more: NYC Homeless Highlight Dangerous Living Conditions