“I credit Callen-Lorde with saving my life,” said Leo, who identifies as a Black gay man and a Callen-Lorde patient for over a decade. After routine lab tests showed early signs of anal cancer, Leo underwent treatment to remove the pre-cancerous cells before they developed into something more serious.
Diana identifies as a Black transgender woman and has been living with HIV for many years. Traditional healthcare providers often shamed and demeaned her so she avoided going to the doctor putting her at higher risk for complications. Since coming to Callen-Lorde she says she can now “trust my healthcare” and even though her access to health insurance has been intermittent, her HIV treatment and routine medical care are now consistent.
“I was at my lowest, and Callen-Lorde accepted me for who I am,” said William a gay man living with HIV who struggled with substance use. William was living in a shelter and felt the future he wanted was impossible. Working with welcoming behavioral and primary health providers, William has found an exciting career path and is now managing his health “like an expert.”
This is the power of inclusive primary healthcare to prevent more severe illness and higher healthcare costs.
Callen-Lorde provides care to patients regardless of their ability to pay. We work with 20,000 patients, many of whom identify as people of color hailing from all five boroughs and beyond. Our patients identify as lesbian, gay, bisexual, transgender or gender nonbinary; about a quarter are transgender.
We are unique in focusing on LGBTQ+ primary care, but we’re just one of a network of community-based health centers across the country that are dedicated to providing whole-person care to vulnerable populations. The 1,400 healthcare centers across the country care for 31.5 million patients in 15,000 communities. We share a history of fighting for inclusive care that encompasses all aspects of health. More preventive care can lower hospital visits, emergency room trips and ultimately costs for both patients and health systems.
However, primary care has been underfunded for decades because insurance companies are stuck in a cycle of paying high prices for acute and emergency care–leaving less for organizations that provide preventive services. Case in point: commercially insured New Yorkers make up 41% of Callen-Lorde’s patient population but only 7% of our patient revenue. As a result, we and other organizations around the U.S. struggle to operate and hire, which can erode care.
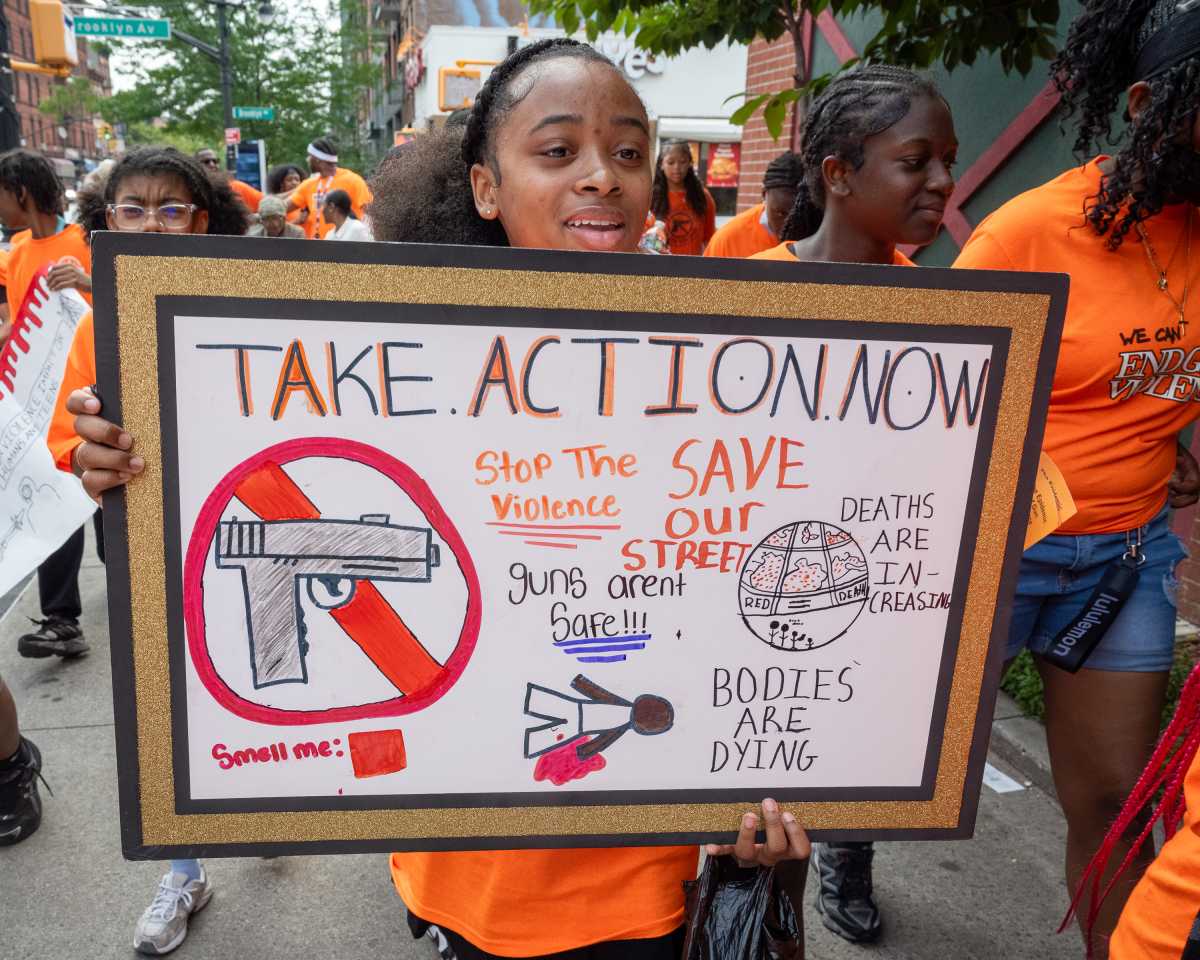
And although primary care is underfunded, patients’ need for it is growing. According to the Primary Care Development Corporation, about 60% of Americans live with a chronic condition that requires consistent management, with people of color and other minority communities, including LGBTQ+ communities, experiencing disproportionately high rates of illness. Complicating things further, many Americans–including 6.5 million New Yorkers–live in areas that have a shortage of primary care health professionals.
This National Health Center Week, Callen-Lorde is using our voice to advocate for more investments in primary care that break the cycle of underfunding.
We recognize that feasible solutions must be incremental. One potential measure is a New York bill that would require all insurers across the state to measure and report the percentage of their overall health care spending that goes toward primary care. The legislation would stipulate that insurers who spend less than 12.5% on such care must increase spending by 1% per year until they hit that number. It would be a relatively small, doable change–but one that would put the state on a direct path to more equitable health outcomes.
We already know that similar legislation works in other states–more than a dozen have adopted such investment measures. Rhode Island mandated commercial insurers to increase investment in primary care by 1% annually over five years in 2009. Between 2008 and 2012, primary care spending grew by 37%–while total medical spending dropped by 14% and more primary care physicians joined the state’s workforce.
Everyone deserves access to equitable preventive care that fosters healthy bodies, minds and communities. The kind of care that Leo, Diana and William receive at Callen-Lorde. But we can’t continue providing it without better investments at all levels of government. We hope you’ll join Callen-Lorde in advocating for incremental change that will have a lasting impact on patients across the city.
Patrick McGovern is CEO of Callen-Lorde Health Center which provides sensitive quality healthcare and other services to New York’s LBGTQ+ community in all their diversity regardless of the ability to pay.
Read More: https://www.amny.com/opinion/